AED Requirements by State in 2025: Updated Compliance Guide for Schools, Gyms, and Businesses
Stay compliant in 2025. Learn AED requirements by state for schools, gyms, offices, and public facilities. Updated laws and guidance to protect lives and avoid fines.
In 2025, many states including Georgia, Texas, Virginia, Massachusetts, and California require AEDs in schools. Laws vary by state, with some covering all K-12 schools and others requiring AEDs at athletic events or campuses only. Most states do not mandate AEDs in all workplaces. However, industries with high risk such as gyms, airlines, and large public venues often face specific AED laws or OSHA-driven recommendations."
Yes. All 50 U.S. states provide some level of immunity for bystanders who use an AED in good faith. These laws are designed to encourage quick action without fear of legal consequences.
Introduction
Sudden cardiac arrest (SCA) strikes without warning—and every minute counts. The American Heart Association estimates survival rates decline 7–10% for every minute a victim goes without defibrillation.¹ Yet, many facilities remain unprepared.
While there is no sweeping federal law mandating AEDs everywhere, states across the U.S. increasingly pass legislation requiring or encouraging AEDs in schools, athletic facilities, workplaces, and public spaces. In 2025, keeping up with evolving state laws is more important than ever—for safety, compliance, and liability protection.
In this guide, we provide a state-by-state snapshot of AED laws (schools, gyms, public access), highlight trends, and share actionable advice to keep your facility ready—whether or not your state mandates an AED.
Why AED Laws Matter in 2025
Life-saving potential. The faster an AED is applied after collapse, the higher the chance of survival.
Liability & legal risk. Failing to provide an AED where required can expose organizations to legal claims.
Public expectation & reputation. Customers, parents, employees, and visitors expect safety measures in modern facilities.
Legislative momentum. New laws, especially in school systems and public venues, are passing regularly (e.g. Georgia’s 2025 requirement for all K-12 schools)
Even in states where AEDs aren’t yet mandated, adopting best practices positions your business or institution ahead of regulation and improves safety.
Federal & National Guidance: OSHA, CDC, and “Good Samaritan” Laws
OSHA & Workplace Programs: OSHA doesn’t mandate AEDs specifically in its standards, but it does encourage organizations to adopt AED programs under first-aid and workplace safety guidelines.
Maintenance & Reporting Requirements: Many states require or encourage routine testing, maintenance, and reporting of AED usage to EMS or state agencies.
Liability Protections (Good Samaritan Laws): All 50 states provide some level of civil immunity for bystanders using an AED in good faith, protecting lay rescuers from liability in most cases.
Taken together, federal and state frameworks encourage readiness, training, and program oversight—even where hard mandates don’t yet exist.
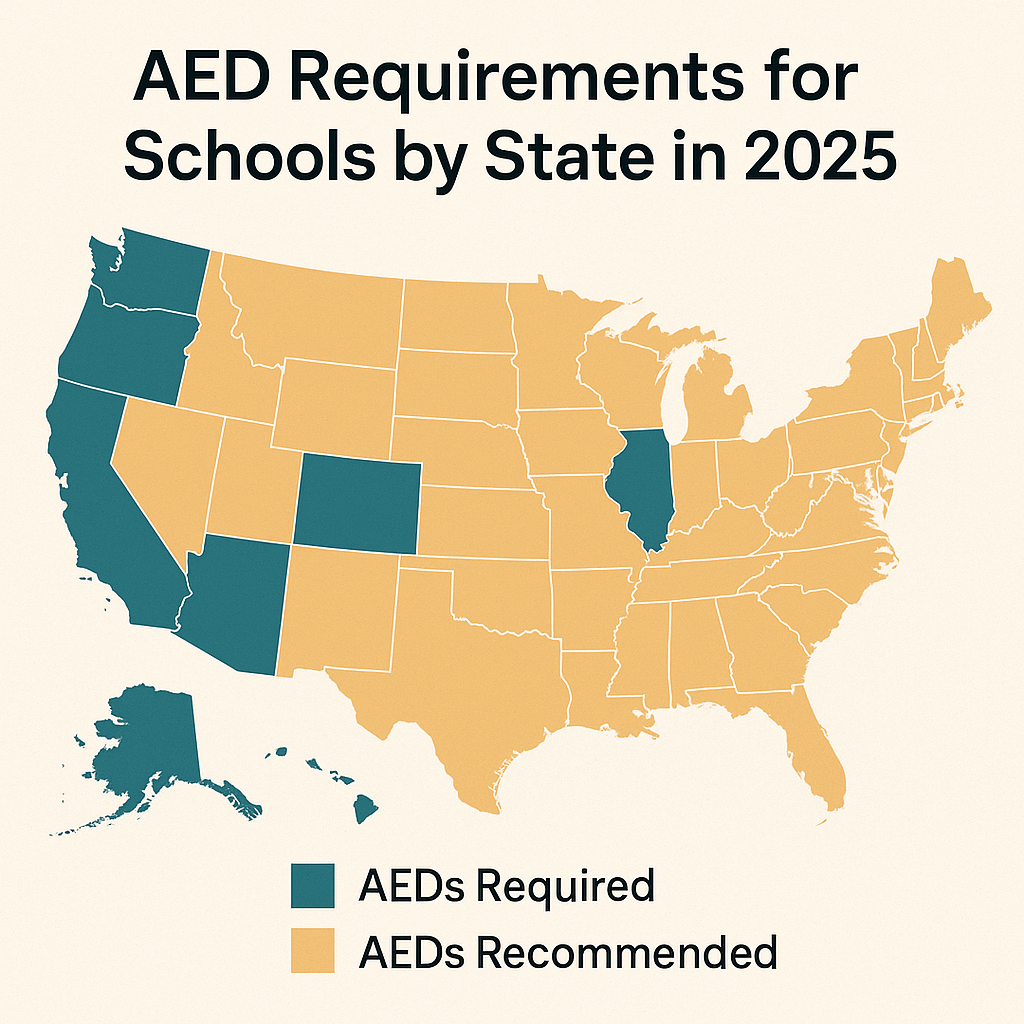
State-by-State Snapshot (2025)
Who Should Install an AED Even If It’s Not Required
Just because your state doesn’t legally require an AED in your facility doesn’t mean you shouldn’t install one. Consider an AED in:
Offices with 50+ employees or high foot traffic
Churches, community centers, and auditoriums
Manufacturing plants, warehouses, or factories
Hotels, shopping centers, event venues
Sports clubs, youth leagues, recreational facilities
Installing an AED proactively improves safety and may give you a competitive or reputational advantage.
How to Stay Compliant & Maintain an AED Program
Even where AEDs are legally required, many organizations fail to remain compliant over time. Use the checklist below to maintain readiness:
Scheduled maintenance & self-tests
Ensure your AED meets manufacturer specs for battery checks, electrode pad expiration, and self-tests. States often require or encourage routine maintenance.AED use reporting & oversight
Some states require that any clinical use of an AED be reported to EMS or medical oversight.Medical direction / oversight
Many AED programs must have a licensed physician or medical authority supervising protocols.Staff training & drills
CPR/AED training for staff (especially first responders) and regular mock drills to test response.Emergency Action Plan (EAP)
Build, document, post, and rehearse your cardiac response plan—include who retrieves the AED, who calls 911, who uses the device, etc.Signage & visibility
Keep AEDs clearly labeled, easily accessible, and known to all occupants.Replace components on schedule
Batteries and electrode pads have limited shelf life—replace before expiration.Annual or semiannual audit
Review every component of your AED program: readiness, logs, staff awareness, signage, medical oversite.
Trends & 2025 Updates to Watch
Expanding school mandates. States like Georgia are broadening school AED requirements to include all K-12 (not just high schools).
Increased CPR/AED Training Laws. New laws (e.g. Texas’s Landon Payton Act) require more school staff to hold current credentials and conduct drills.
Focus on accountability & reporting. Many states now require use-reporting, program audits, and integration with EMS.
Grants & funding push. Federal grants (like via the HEARTS Act) encourage schools and non-profits to adopt AEDs and emergency response plans.
Conclusion & Call to Action
In 2025, being proactive with AED readiness is no longer optional—it’s essential. Whether your state requires an AED or not, a well-implemented AED program elevates safety, protects your organization, and positions you ahead of regulation.
If you’d like help choosing the right AED package, managing maintenance, or designing a full AED program for one or multiple sites, AED Pro is here to help. Contact us for a free compliance consultation and let’s make your facility a safer place.